THE ULTIMATE BEGINNER'S GUIDE TO FEMALE PELVIC PAIN (CPPS)
Written By: Dr. Brianne Grogan, PT, DPT
Fear. Shame. Guilt. Grief. Anger. Burden. Avoidance. Withdrawal. Too many women suffer in silence with persistent pelvic pain, which can lead to any (or all) of the emotions just listed. The good news is that you are not alone, you are not making this up, and there is help for you! In this guide, I will share information about chronic pelvic pain syndrome, explain terms you might have heard including vulvodynia, vaginismus, and dyspareunia, introduce basic anatomy to better understand your body, identify potential root causes, and provide simple steps you can begin today.
MY LIFE-CHANGING EXPERIENCE WITH PELVIC PAIN
When I first started working in the field of pelvic floor physical therapy, I was shocked by the sheer number of women who had debilitating pelvic pain. About 50% of my clients came in for issues such as bladder leakage and/or prolapse, and the other half were at their wits’ end due to extreme pain during intercourse (dyspareunia) and/or involuntary tightening of the pelvic floor muscles during sex or any type of vaginal penetration (vaginismus).
These women’s bodies were in discomfort, but what struck me most strongly was the emotional/mental discomfort that my patients were experiencing; it was despair, in fact.
My patients were all ages – and the reasons for their pain varied – but in almost all cases their intimate lives were significantly impacted and they felt exasperated, angry, and embarrassed by their inability to enjoy pain-free sex. My clients with dyspareunia often felt obligated to have sex for the sake of their partner even though they dreaded the experience, and afterward felt ashamed and defeated that “it didn’t work… yet again.”
Countless patients told me that their doctors told them, “it’s all in your head,” or that the condition would resolve on its own. They were often told to “drink a glass of wine, close your eyes, and get it over with” – a patriarchal view that dismissed the woman (and her enjoyment) from the equation altogether.
This dismissive attitude fired me up and made me passionate about helping women find natural solutions for their pain!
One client that I’ll never forget was a newlywed. She and her husband had not had sex before marriage, and she was distraught by the fact that they’d been married for 6 months and had not been able to consummate their marriage due to her extreme vaginismus. She desperately wanted an intimate connection, and she also wanted to have a baby.
My client and I worked on relaxation exercises for her pelvic floor muscles, and later we brought in her husband to assist with gradually progressive re-exposure exercises to relax her pelvic muscles and calm her nervous system. We also explored dilator therapy.
After several sessions, she started to improve and stopped coming in for treatments. About a year later, she returned to the clinic with her newborn baby in a carrier. She said, “I couldn’t have done this without you!” I cried tears of joy, realizing that this work is truly life-changing. Because of my client’s dedication to resolving her chronic pelvic pain and bravely seeking treatment, she was able to overcome vaginismus and enjoy a satisfying intimate life with her partner… and conceive a baby!

WHAT IS FEMALE CHRONIC PELVIC PAIN SYNDROME?
Chronic Pelvic Pain Syndrome (CPPS) is a broad term used to describe persistent pain in the pelvic region that may be attributed to a variety of root causes. In women, CPPS is defined as “persistent, noncyclic pain perceived to be in structures related to the pelvis and lasting more than six months.” Unfortunately, CPPS is often left untreated since many women are embarrassed to talk about it, ashamed of their condition, or left to think that it’s “normal” for sex to hurt (among other symptoms).

CPPS is a mystery to many healthcare providers because the symptoms can vary widely and the cause is often unclear. In some women, CPPS can appear to “spring up” out of nowhere (unknown etiology); however, the following is a list of possible contributing factors:
- traumatic injury such as car accidents or falls
- injuries sustained during pregnancy or childbirth
- scar tissue and/or adhesions due to injuries or surgery
- a history of painful periods or endometriosis
- a history of chronic urinary tract infections or yeast infections
- interstitial cystitis (painful bladder syndrome)
- psychological trauma, or a history of physical or sexual abuse
- chronic stress, anxiousness, or fear/protective mechanisms that are in “overdrive”
- habitual ways of holding self due to work or leisure (posture)
- hypermobility of the joints which leads to gripping of the pelvic floor to help stabilize
- bladder leakage or pelvic organ prolapse which leads to unconsciously gripping the pelvic floor in an effort to “hold everything in”
Often, CPPS it the result of one or more of these issues and the net result is tense, overactive pelvic floor muscles. This tension in the pelvic muscles is one reason CPPS is sometimes referred to as levator ani myalgia. Levator ani myalgia is characterized by hypertonic and shortened pelvic floor muscles, often with tender points.
This pelvic tension and pain often goes hand-in-hand with digestive issues, bladder concerns (like frequency or urinary hesitancy), and back pain. In fact, recent studies have shown that more than 95% of women with low back pain have pelvic floor dysfunction as well [1].
CPPS can be a “chicken or the egg” scenario; for example, did back pain lead to pelvic tension, or did pelvic tension lead to back pain? It can be a mystery that’s difficult to unravel, but as you’ll see, a comprehensive holistic treatment plan WORKS, and awareness is the first step!

Free Masterclass: How to Heal Pelvic Pain Naturally
Whether you’ve had pain for years or just started feeling like something’s not right, this masterclass with Dr. Bri will help you understand what’s going on and give you hope that healing is possible.
SPECIFIC PAIN DIAGNOSES
Men can have CPPS too, but the following specific pelvic pain diagnoses are only seen in individuals with female genitalia:
-Vaginismus
Vaginismus is when the vaginal muscles (and the muscles surrounding the vagina) involuntarily or persistently contract when vaginal penetration is attempted. This can include times such as sexual intercourse, gynecology appointments, and tampon insertion.
Women with vaginismus should NOT be doing Kegel exercises. Rather, they should seek the care of a women's health physical therapist to work on relaxation/release instead. Techniques such as manual therapy, EMG biofeedback, and various methods of pelvic floor "down-training" must be done BEFORE beginning any type of "up-training" (strengthening) program.
-Vulvodynia and Vestibulodynia
Vulvodynia is pain or discomfort in the vulva – the area including and surrounding a woman's genitals – that is not due to a clear identifiable cause (such as infection or a skin disorder). The pain is often described as raw, burning, itching, or stinging.
In some people with vulvodynia, the pain only occurs when provoked (for example, by touch, tampon insertion, wiping after using the toilet, or wearing underwear or tight clothing). For others, the pain is classified as “unprovoked,” meaning that it can appear anytime. The pain can be generalized, or localized to certain areas such as the clitoris or the vaginal entrance.
As indicated by the image below, it can feel like a ring of fire:

The vaginal entrance is known as the “vestibule.” Vestibulodynia is the most common type of vulvodynia, and is defined as chronic pain and discomfort that occurs specifically around the opening of the vagina, inside the inner lips of the vulva.
Both vulvodynia and vestibulodynia can be treated with physical therapy, and other suggestions such as those found in this guide. Topical medications may also be prescribed.
Do Tight Pelvic Floor Muscles Cause Vulvodynia and Pelvic Pain?
Pelvic pain disorders of all types are usually associated with pelvic floor overactivity. Increased tone causes a decrease in blood flow (and therefore, a decrease in oxygen and nutrients) to and from the muscles of the pelvic floor. Decreased circulation also makes it harder for waste products, such as lactic acid buildup, to “escape.” Therefore, tight pelvic floor muscles can cause pain. This pain – in turn – may make your pelvic floor tighter, and vulvodynia symptoms feel more intense.
COMMON SYMPTOMS
Pelvic Floor Dysfunction or CPPS (Chronic Pelvic Pain Syndrome) are blanket terms that describe lack of normal functioning in your pelvic floor muscles and organs. There are a wide range of possible symptoms, and these symptoms can shift and change over time. Common symptoms of CPPS include:
- Tightness in the perineum (the area between the vagina and the anus); can feel like a “knot” of tension
- Aching, burning, tightness, spasming, or numbness in vulva and/or pelvic region
- Difficulty letting go after a pelvic floor contraction (Kegel)
- Kegel exercises make symptoms WORSE
- Spasms can be felt in the vaginal area, or in the rectum (referred to as proctalgia fugax)
- Burning, shooting, or prickling nerve pain in the “saddle region” (pudendal neuralgia)
- Urinary frequency and/or urgency
- Feeling like you "always have to go pee"
- Pain during sex and/or tampon insertion
- Pain during or after bowel movements
- Pain while sitting
- Pain in the pelvic area during or after exercise
- Lower abdominal pain
- Low back pain
The emotional and mental symptoms associated with CPPS cannot be overstated. Depression and anxiety go hand-in-hand with CPPS, and may contribute to its onset as well as perpetuate it (make it continue, and make it feel more intense).
ANATOMY OF YOUR PELVIC FLOOR
The pelvic floor muscles are found at the base of your pelvis. They create a “hammock” of support that slings from the pubic bone in the front, to the tailbone in the back, and between the sitting bones from side-to-side.
To keep things simple, there are layers to your pelvic floor: a deep inner layer with a group of muscles that collectively make up the levator ani (which literally means “anus lifter”), and an outer layer of smaller, more superficial muscles that surround your anus in the back and your vagina and urethra in the front. Together, the pelvic floor muscles help support your internal organs, provide core stability, and contract and relax to help with bowel and bladder function, childbirth, and sex.
You can see a diagram of the inner female pelvic floor muscles below:

This image shows what the outer layer of muscles looks like:

Your pelvic floor muscles can help you experience pleasure, and they can also contribute to pain. Let’s talk a little bit more about pain.

POTENTIAL ROOT CAUSES
As stated by Dr. Greg Lehman, “pain is weird, and pain is influenced by a number of factors.”
There is not just one root cause, but many factors that can contribute to CPPS. In this section, I will cover some potential root causes to take into consideration. This is not intended to be a substitute for medical evaluation or treatment and is certainly not a diagnosis, but it can help open your mind to the possibilities of what could be causing your pain. Awareness is the first step to relief!
Pelvic Floor Tension
Excessive pelvic floor tension can contribute to pelvic pain. The next section (Nervous System Dysregulation) explains one reason why this buildup of tension can happen.
Nervous System Dysregulation
In my opinion, the most important potential root cause to highlight is nervous system dysregulation; specifically, over-activation of the stress response and pain signaling pathways. We see it time and again with people who have CPPS.
Our mind and emotions are intimately connected to what’s physically happening in the body. There is constant two-way communication between our brain and body, and we unconsciously, automatically, and reflexively create tension in our tissues simply by the thoughts we think (whether or not we’re even aware of these thoughts).
What’s one of the first places in the body to automatically “tense up” in response to stressful thoughts? The pelvic floor!
Your body is designed to activate the protective fight/flight/freeze response whenever you encounter danger. In this modern day, we often confuse fear with danger. Danger is an immediate threat to your body whereas fear is a psychophysiological experience, caused by a thought.
Chronically thinking fearful thoughts, reacting with a stress response, and worrying too much about the future or attempting to control it (anxiety) will throw your nervous system into a high-alert, upregulated state. Your pelvic floor is a part of your body and goes into “brace mode” in response to the fear and uncertainty of everyday life – including what’s going on in the news, what’s happening at work, family concerns, etc. It tenses up and holds this tension, as your body prepares to fight, flee, or freeze. This is what your body is designed to do, to protect you! But when we maintain this state for too long, without being aware of it (which can happen in this super-fast paced, pressure-filled modern life), then problems such as CPPS can arise.
With CPPS, a tension-pain cycle develops which looks something like this: pelvic tension causes pelvic floor dysfunction which causes stress, fear, embarrassment, and uncertainty. This sends danger messages to your brain, increasing your internal “alarm bells” and pain sensing mechanisms. Your brain’s response to the “danger alarm” is to create pain, which causes more tension in the body (including the pelvic floor), and more pain. Over time, with repeated input, these stress and pain responses become super-sensitive and this cycle happens faster and faster, with smaller and smaller inputs needed to make the alarm bells sound. This is called “central sensitization.”
It’s important to know that you haven’t done anything wrong… your body is only trying to protect you by “turning up the volume” on the alarm system! Pain pathways are created over time, and they can be CHANGED over time as well. Awareness of the tension-pain cycle is the first step to interrupting it by down-regulating, or calming, your nervous system.
Direct Injury
Injuries in the pelvic region are surprisingly common among women. In addition to the possibility of sustaining a fall, or being involved in an accident that causes direct injury to the coccyx (or somewhere in the pelvic area), many women sustain injury during childbirth. A large-scale study of vaginal deliveries found that the majority of women (78%) undergoing childbirth had a tear, and 47.1% suffered from perineal lacerations [2].
A more recent study reported that levator ani muscle avulsion (detachment of muscle from bony insertion) occurs in approximately 15% to 30% of first vaginal deliveries, and external anal sphincter defects in up to 25% [3].
Birth-related pelvic floor trauma is associated with higher rates of postnatal depression, and can have long-term impacts on health and quality of life.
Injury of any sort – birth-related or not – can contribute to acute inflammation (which can cause pain and patterns of muscular holding), and if the injury causes nerve damage or a wound, then longer-term challenges might arise such as weakness or scar tissue resulting in soft tissue restriction and/or patterns of misalignment.
All of these aspects can contribute to pain.
Body Misalignment
The tension-pain cycle discussed above can cause poor postural alignment, sitting habits, and lack of movement which can “feed” the cycle and just make things worse! But even aside from the pain-tension cycle, chronic alignment issues cause patterns of restriction and holding in your tissues. If you spend most of your day slouched in front of the computer at work and then sit on the couch scrolling through Instagram after dinner, then you’re spending most of your day in an unhealthy position that tightens certain muscles and lengthens others.
It’s not that sitting is “bad,” but you DO want freedom of movement and lots of different options. Humans were built to have a huge amount of variability in movement, and when we get stuck repeating certain patterns, we suffer. Overly tight muscles aren’t strong. Overly-lengthened muscles aren’t strong. These imbalances lead to weakness, and ultimately pain and dysfunction.
Motion is lotion! Learn how to gradually return to pain-free movement in our FREE MASTERCLASS
Improper Nutrition and Constipation
A diet that lacks balance can lead to inflammation, digestive tract issues, and constipation. Constipation and an unhealthy gut can cause tension which pulls and impacts your pelvic floor functionality, including pain with bowel movements.
Furthermore, constipation and straining to “go” can contribute to hemorrhoids (piles) and can lead to prolapse over time. The remedy? Eat more plants and drink more water!
Medical Concerns
Some cases of pelvic pain are, in fact, caused by a bacterial infection, a sexually transmitted infection, or a significant medical concern such as cancer. This is not meant to induce fear, it’s simply to say that while a holistic mind-body approach and conservative treatment options (such as movement, lifestyle, and/or physical therapy) can be helpful for most cases of CPPS and pelvic floor dysfunction, it’s VERY IMPORTANT to rule out a medical concern that may require more aggressive treatment. Talk to your doctor, get testing, and be sure they rule out any red flags such as warmth or redness that may indicate infection, burning pain, radiating numbness or tingling, sudden changes in bowel or bladder habits, sudden changes in weight or appetite, and changes in balance or ability to walk.

Stop Doing Kegels…For Now
Years ago, the prescription for everyone who had pelvic floor dysfunction of any type (pain, bladder leakage, prolapse, painful sex, etc.) was to “do Kegel exercises.” Today, we know better!
Kegel exercises – which are exercises that contract and relax the pelvic floor in isolation – are not appropriate for all individuals, and they’re typically NOT a good starting place for people with pelvic pain. Tight muscles are tired muscles; thus, the first focus needs to be on relaxation, release, and mobility.
Tight muscles are also weak muscles, so they will need gradually progressive strengthening (which may include Kegel exercises as part of a well-rounded total core strengthening program) …but initially, they need to rest and release!

Daily Movement to Relax and Release Your Pelvic Floor
“If it hurts, don’t do it” is totally reasonable for short-term acute pain, but it’s not helpful long-term! Movement is medicine, and you don’t need “fixing” before you start doing.
There’s a beautiful balance between the “no pain no gain” approach (pushing too hard) and avoiding things altogether. Exercise is an analgesic. It helps with pain. It calms things down. It makes you happier. It makes you healthier! And it’s ONE PART of the solution to the larger puzzle.
It is important that you integrate daily movements which are designed to release and relax your pelvic floor muscles and the surrounding muscle groups. The Overcome Pelvic Pain for Women program has a scientifically designed routine for 12 weeks in a row, taking the guesswork out of this.
Whether you are following a set of individualized routines from your physical therapist or following the Overcome Pelvic Pain program, make sure to stay consistent with your daily exercises. Initially, it is important to downtrain your pelvic floor muscles, which means to bring them to a place of neutrality, without constant tension. Later on, you will want to begin re-strengthening the surrounding muscles groups, and ultimately regain coordination and control within the pelvic floor itself — which is what our 12 week build-up does in the Overcome program.
You might feel some soreness and discomfort for the first few days or even weeks, as you begin to unclench these chronically tight muscles. This is normal, as you begin to “wake up” muscles that haven’t been moved in such a way in perhaps a very long time. Your body is fighting to “stay in the past,” but don’t let your body take over your mind! Start slow, and the body and your pain protective system will adapt. Come back into balance by breathing deeply, releasing fears, going slow, and being consistent with your daily movement routine.

Free Masterclass: How to Heal Pelvic Pain Naturally
Learn my favorite rhythmic breath and movement techniques for pain relief in my free masterclass!

A Clean Diet
Your nutritional intake is significantly more important when it comes to pelvic tension than you might have realized. Your gut health influences your entire body’s chemistry, and has a lot to do with the regulation of your nervous system. Not to mention, that an overly worked, stopped up, and constipated digestive tract can lead to exacerbated pelvic floor tension and symptoms.
Consider greatly reducing your intake of sugar, alcohol, caffeine, and other stimulants while doing the Overcome program or your own recovery program. These substances can create inflammation and irritation in the bladder and pelvic regions.
Crowd out unhealthy, greasy foods with more whole foods. The more you can eat real food (in other words, food that doesn’t come from a box or can or bag), the more vibrancy and digestibility you will bring into your diet! Healthy fats such as olive oil and avocado, lean protein sources, vegetables, fruits, legumes, nuts, and some grains work well for most people. Every BODY is different, so you will need to discover your own bio-individuality regarding nutrition intake. The Overcome Pelvic Pain program includes nutritional guidance for each month of your recovery program, to make this easy to understand and follow.

Bringing Safety Into Your Nervous System
In the words of one of my mentors, “if you’re dealing with pelvic issues, you’re dealing with trauma.” Trauma is any unresolved issue that remains “stuck” in the body. Whether a trauma contributed to the development of your CPPS, or your CPPS resulted in the traumatic experience of being misdiagnosed and misunderstood… you likely are holding onto trauma.
The remedy is to create safety in your mind, body, and environment. Give yourself time, space, privacy, and a comfortable environment in which to do your exercises. Tell your family and/or your housemates that you need a few minutes every day to do some self-care. Light a candle, play some soft music, or diffuse your favorite calming essential oil while moving and stretching. Anything you can do to reduce signals of potential danger and increase signals of SAFETY in your mind and body will add to your healing process.

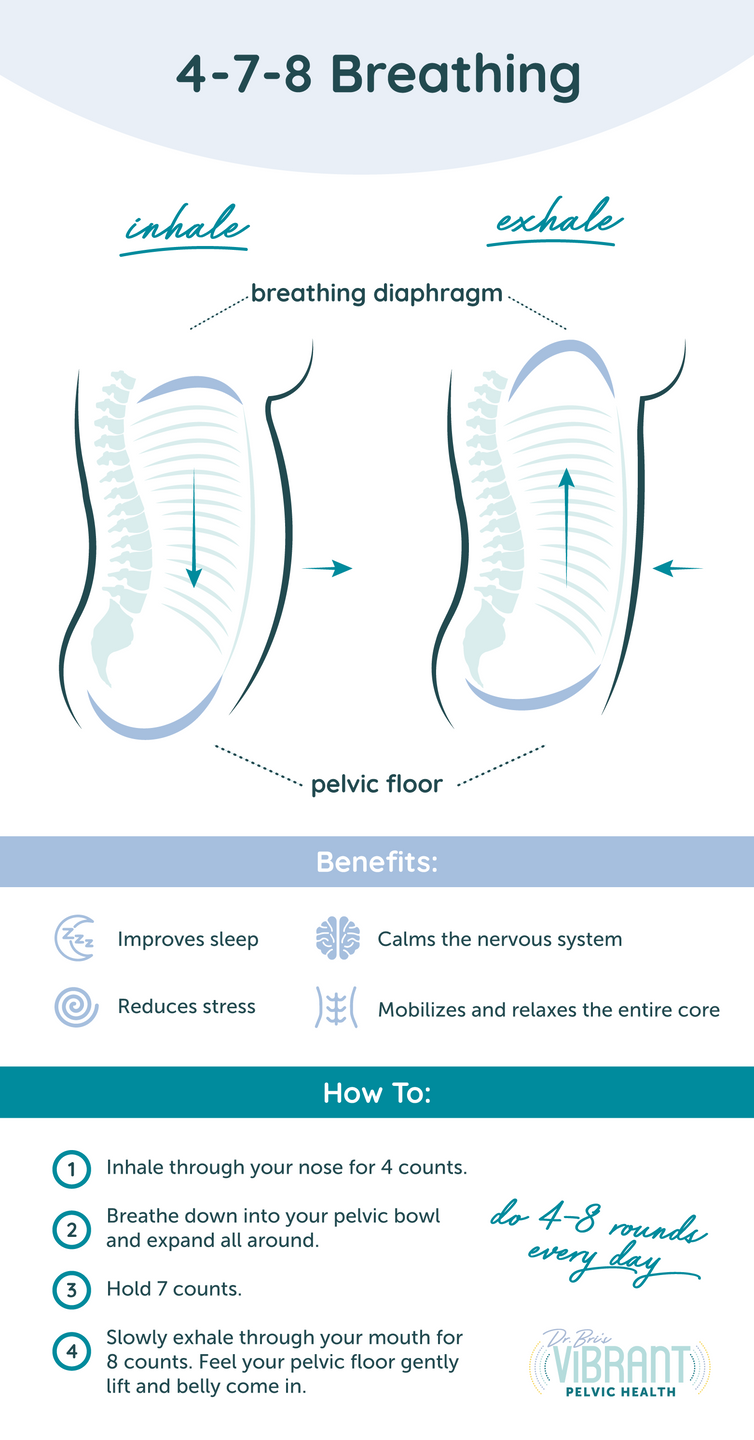
A calming breath pattern that stimulates the relaxation response (via the vagus nerve) is called the 4-7-8 breath. It induces a feeling of calm and safety, and can also help with sleep. Begin by exhaling all of your air out. Then inhale through your nose for 4 counts, suspend your breath for 7 counts, and exhale out your mouth for 8 counts. Repeat for 4 breath cycles.

The Importance of Mind-Body Practices
Your mindset can keep you stuck or it can liberate you. One shift is moving into gratitude. Even if you feel pain, even if it looks as though things are not changing, what can you find gratitude for right now? True gratitude opens your heart and leads to harmonious function throughout your entire body.

Another shift is living in the present moment. When you stop ruminating on the past and worrying about the future, you are fully present. You will not be able to experience anxiety and stress when you are fully present in the “now,” which is highly beneficial for downregulating your nervous system (and ultimately, for healing).
It's also important to monitor your self-talk. Any thoughts that you think or say to yourself on repeat have a tremendous (and measurable) effect on your body's physiology. The emerging science of psychoneuroimmunology is showing us the unbelievable power of the human mind. Your mind can and does influence your body. What does this mean? If cyclical, negative thoughts and emotions can make you sick, that means that conscious, positive thoughts can make you healthy (along with the other mechanical and chemical changes in unison).
Consider: How are you speaking to yourself? What words and thoughts are you “feeding” yourself day in and day out?
You can begin retraining your brain, wiring and firing new neural networks together. You have been walking down the same (neural) path over and over again, which is that which leads to the experience of chronic pain. The path has become a multi-lane highway! You will need to "wire and fire" new neurons together, creating new thought pathways of health, wholeness, and function. This neurologically reprograms your nervous system back into health.
How is this done? There are many ways. One is new information. Reading, listening to, and experiencing knowledge and possibility, creates new belief systems. Then, doing practices such as affirmations, guided meditations, and mindful breathing, brings your “learning” from the mind into the body! All of this is integrated into the Overcome Pelvic Pain program for you. The program includes a guide on how the mind-body practices change your brain and body, along with a library of custom-designed meditations and mind workshops, which are for subconscious reprogramming.
A Support System
You don’t have to do this alone. Research has found that the strength of one's social support network has a significant impact on physical and mental health outcomes after illness or injury [4].
–Family and Friends
You don’t want to be a broken record about your chronic pain, but let others know what you are doing to actively help your health. Set boundaries when needed. Advocate for help, if required, so that you can complete your daily stretches and self-care practices. Others will begin seeing the NEW YOU, and not the past you, as you begin to take steps toward recovery and begin to shine again!
–Community
Joining an online or local community of people who are recovering together can be super-supportive. In the Overcome Pelvic Pain program, we have a private online community that’s just for the women in the program, where my team and I assist by answering questions and giving powerful support.
Don’t be afraid to speak up and ask for help and to share your own wisdom with those around you; everyone has a gift to give!
–Practitioner/Coach/Guide
Finding an experienced practitioner, such as a physical therapist (or another related health professional) can be very helpful. You can also enlist a coach or guide to be there for you along the way, giving you support on your beautiful journey of recovery back to strength. I’d love to be that guide for you. It is my life’s purpose and passion to help women overcome their pelvic health challenges and get back to living a vibrant life!

Finding Joy in the Now - You’re More than Your Pelvic Floor
Your diagnosis does not define you! You are so much more than your pelvic floor. It can be easy to get caught up in your symptoms and forget about having fun when you are experiencing CPPS. A little-known secret is finding joy every day, but it has to be personalized to you. >> What is meaningful to YOU, that you’ve been missing out on?
One of the most profound and important questions you can ask yourself is: “what would I be doing if my pain was less of a problem for me?”
Even while you are recovering, what can you do today that will bring you joy? And then see how you can ease into it.
Just remember: as you slowly ease back into your favorite activities, you might experience some flares of pain or muscle soreness. But pain can be a poor guide. Hurt does not always equal harm! Gradually and gently poking into mild discomfort and doing the things that are meaningful to YOU helps to turn down the sensitivity of the “pain alarms” that are often on high alert with CPPS.
Maybe you are not able to go on a 10-mile hike, but can you read an adventurous book? Can you walk around the block? What about playing a game with your kids? Or painting? Or dancing to your favorite song? When you lean into joy, and you take your mind off of the problem, your body and mind have the space they need in order to “do their thing.” Don’t wait until you are healed to be joyful. Joy is a powerful choice that you can make, today!
Final Words of Advice:
Just like every person is different, so too is every HEALTHCARE PROVIDER. If you are not satisfied with the evaluation or examination you receive from one provider, then don't be afraid to seek a second opinion.
Advocate for yourself! If you feel like something is "off" in your body, then LISTEN. If you feel blown off by a provider who says your prolapse is "normal" and just something you have to live with, then find someone else who can help.
This guide is not a substitute for individualized medical treatment; contact a physician and/or physical therapist in your area for one-on-one evaluation and a personalized treatment plan.
Sending light and love… and don’t forget to begin the 7 Day Free Kickstart to Recovery!

Dr. Brianne Grogan, PT, DPT
With over 20 million views (and counting) on YouTube, articles featured on MindBodyGreen, courses on DailyOM, and a 5-star reviewed podcast and book, Brianne Grogan is a leading voice in the field of pelvic health and wellness. She is loved by her viewers for her down-to-earth, compassionate approach and for making pelvic floor fitness fun, mainstream, and accessible.

Free 7 Day Kickstart to Overcome Pelvic Pain
Now that you have read this detailed guide, are you ready to put pelvic pain in your past? I created a 7 Day Kickstart which guides you day-by-day with exactly what to do. This kickstart is designed to give you relief as you learn the basics of the Overcome Pelvic Pain for Women program. This is completely free. I want you to get started on the right foot. You can do this, and I can help! Get started right here.
REFERENCES
- Association between lumbopelvic pain and pelvic floor dysfunction in women: A cross sectional study. PMID: 29268147 DOI: 10.1016/j.msksp.2017.12.001
- A prospective observational study on tears during vaginal delivery: occurrences and risk factors. PMID: 11942886, DOI: 10.1046/j.0001-6349.2001.10182.x
- The Importance of Information: Prenatal Education Surrounding Birth-Related Pelvic Floor Trauma Mitigates Symptom-Related Distress. DOI: 10.1097/JWH.0000000000000229
- Perceived social support is strongly associated with recovery after injury. DOI: 10.1097/TA.0000000000003230
How else may we help?
Vibrant Pelvic Health programs are not a substitute for individualized medical treatment; contact a physician and/or physical therapist in your area for one-on-one evaluation and a personalized treatment plan.